Pulse
Pulse
Pulse refers to the pressure wave that expands and recoils arteries when the left ventricle of the heart contracts. It is palpated at many points throughout the body. The most common locations to assess pulses as part of vital sign measurement include radial, brachial, carotid, and apical areas as indicated in the picture below.
Common Pulse Assessment Locations 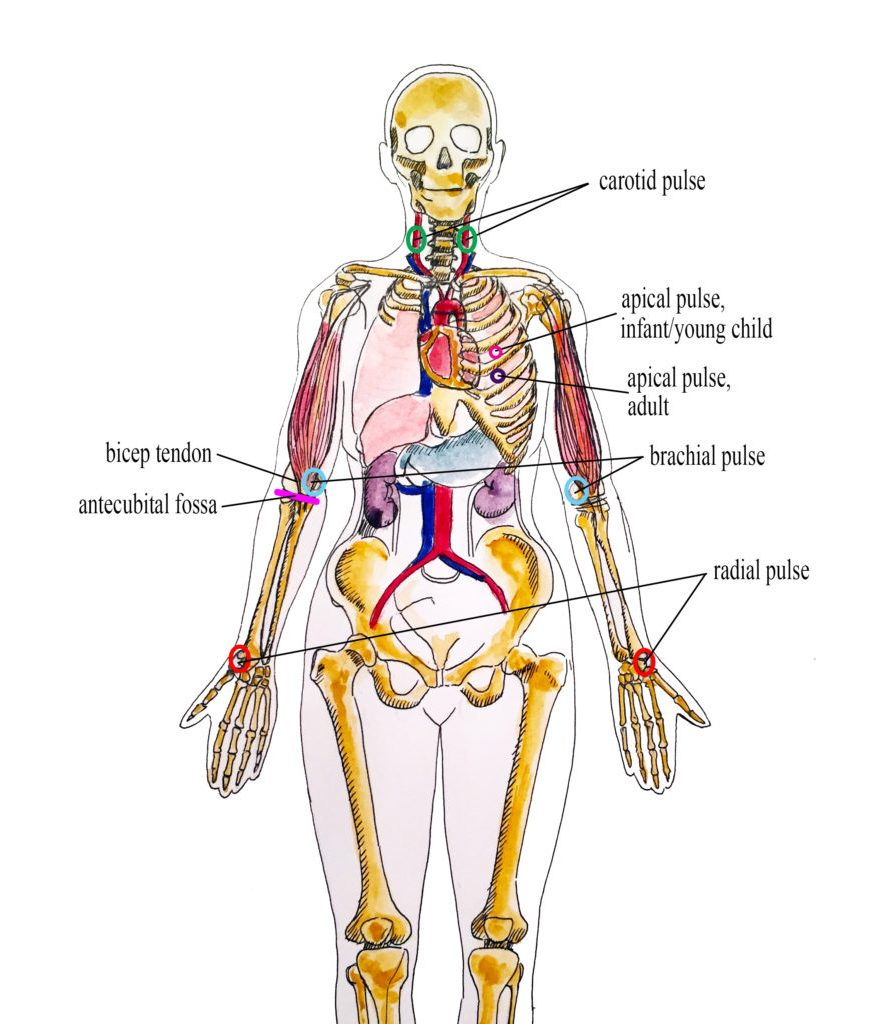
Pulse is measured in beats per minute. The normal adult pulse rate (heart rate) at rest is 60–100 beats per minute with different ranges according to age. The pulse rate is a measurement of the heart rate or the number of times the heart beats per minute. Pulse can be measured wherever a pulse can be palpated whereas a heart rate is auscultated. The pulse rate may differ from the heart rate if the force of the heart contraction is not strong enough to generate a pulse. See Table 1.3b for normal heart rate ranges by age. It is important to consider each patient situation when analyzing if their heart rate is within normal range. Begin by reviewing their documented baseline heart rate. Consider other factors if the pulse is elevated, such as the presence of pain or crying in an infant. It is best to complete the assessment when a patient is resting and comfortable, but if this is not feasible, document the circumstances surrounding the assessment and reassess as needed. For example, pulse rate may be artificially elevated when individuals experience physical or mental stress. Therefore, it is best to collect a pulse rate assessment when the patient is resting.
Normal Heart Rate by Age
Age Group | Heart Rate |
Preterm | 120 – 180 |
Newborn (0 to 1 month) | 100 – 160 |
Infant (1 to 12 months) | 80 – 140 |
Toddler (1 to 3 years) | 80 – 130 |
Preschool (3 to 5 years) | 80 – 110 |
School Age (6 to 12 years) | 70 – 100 |
Adolescents (13 to 18 years) & Adults | 60 – 100 |
When assessing pulses, the characteristics of rhythm, rate, force, and equality are included in the documentation.
A normal pulse has a regular rhythm, meaning the frequency of the pulsation felt by your fingers is an even tempo with equal intervals between pulsations. For example, if you compare the palpation of pulses to listening to music, it follows a constant beat at the same tempo that does not speed up or slow down. Some cardiovascular conditions, such as atrial fibrillation, cause an irregular heart rhythm. If a pulse has an irregular rhythm, document if it is “regularly irregular” (e.g., three regular beats are followed by one missed and this pattern is repeated) or if it is “irregularly irregular” (e.g., there is no rhythm to the irregularity).
The pulse rate is counted with the first beat felt by your fingers as “One.” It is considered best practice to assess a patient’s pulse for a full 60 seconds, especially if there is an irregularity to the rhythm.
The pulse force is the strength of the pulsation felt on palpation. Pulse force can range from absent to bounding. The volume of blood, the heart’s functioning, and the arteries’ elastic properties affect a person’s pulse force.
Pulse force is documented using a four-point scale:
- 3+: Full, bounding
- 2+: Normal/strong
- 1+: Weak, diminished, thready
- 0: Absent/nonpalpable
- Use the pads of your first three fingers to gently palpate the radial pulse.
- The pads of the fingers are placed along the radius bone on the lateral side of the wrist (i.e., the thumb side).
- Fingertips are placed close to the flexor aspect of the wrist (i.e., where the wrist meets the hand and bends).
- See picture below for correct placement of fingers in obtaining a radial pulse.
- Press down with your fingers until you can feel the pulsation, but not so forcefully that you are obliterating the wave of the force passing through the artery.
- Note that radial pulses are difficult to palpate on newborns and children under the age of five, so the brachial or apical pulses are typically obtained in this population.
Radial Pulse

The carotid pulse is typically palpated during medical emergencies because it is the last pulse to disappear when the heart is not pumping an adequate amount of blood.
- Locate the carotid artery medial to the sternomastoid muscle, between the muscle and the trachea, in the middle third of the neck.
- In order to palpate the carotid, place the index and middle fingers on the client’s neck to the side of individual’s trachea.
- With the pads of your three fingers, gently palpate one carotid artery at a time so as not to compromise blood flow to the brain.
- See picture below for correct placement of fingers in a seated patient.
Carotid Pulse

A brachial pulse is typically assessed in infants and children because it can be difficult to feel the radial pulse in these populations.
- The brachial pulse is located by feeling the bicep tendon in the area of the antecubital fossa.
- Move the pads of your three fingers medially from the tendon about 1 inch (2 cm) just above the antecubital fossa.
- It can be helpful to hyperextend the patient’s arm to accentuate the brachial pulse so that you can better feel it.
- You may need to move your fingers around slightly to locate the best place to accurately feel the pulse.
- You typically need to press fairly firmly to palpate the brachial pulse.
- See picture below for correct placement of fingers along the brachial artery.
Brachial Pulse 
The apical pulse rate is considered the most accurate pulse and is indicated when obtaining assessments prior to administering cardiac medications. It is obtained by listening with a stethoscope over a specific position on the patient’s chest wall.