Preventing Infection
Preventing Infection
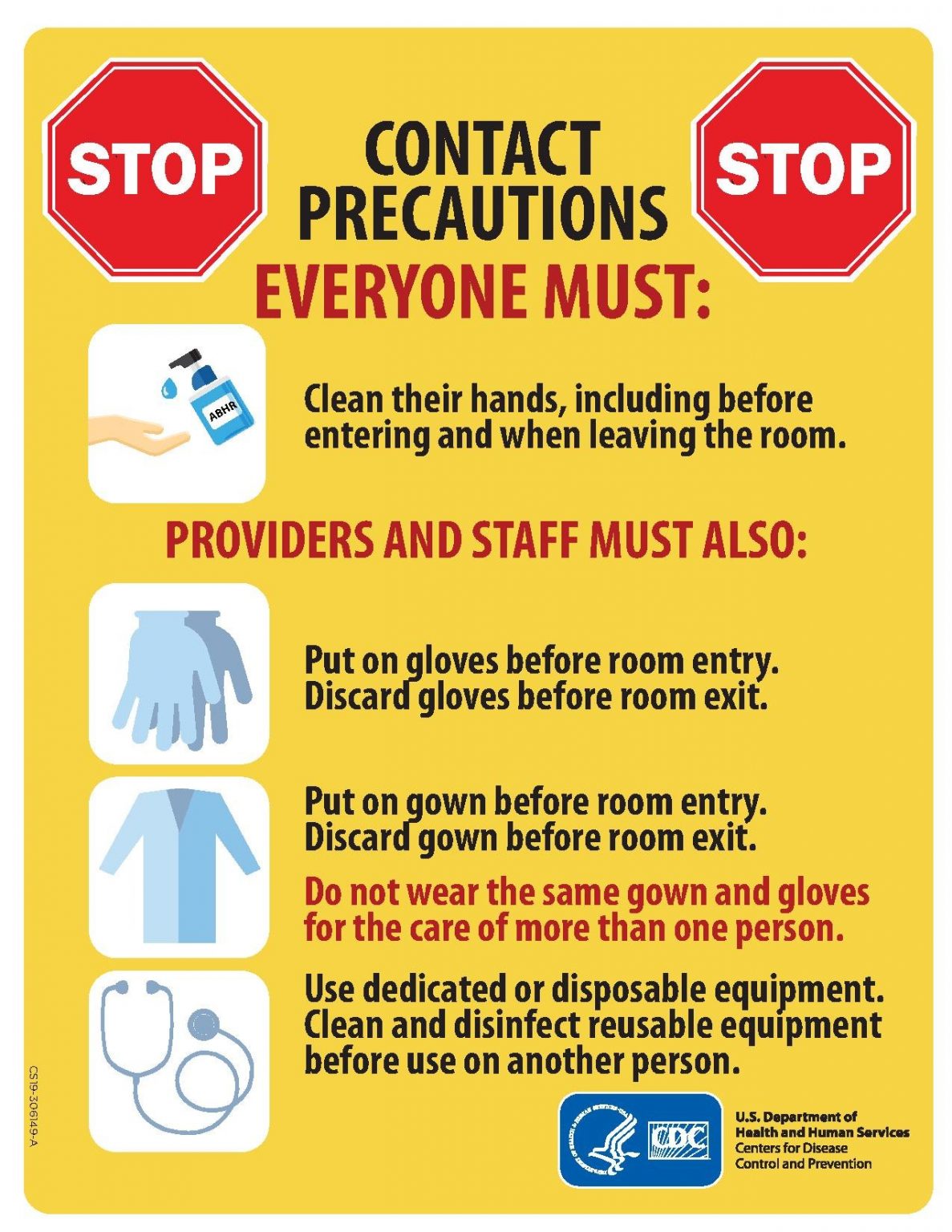
Medical assistants play an important role in preventing the spread of infection. A cyclic process known as the chain of infection describes the transmission of an infection. By implementing interventions to break one or more links in the chain of infection, the spread of infection can be stopped. See the picture below of the links within the chain of infection.
Chain of Infection
- Infectious Agent: A causative organism, such as bacteria, virus, fungi, parasite.
- Reservoir: A place where the organism grows, such as in blood, food, or a wound.
- Portal of Exit: The method by which the organism leaves the reservoir, such as through respiratory secretions, blood, urine, breast milk, or feces.
- Mode of Transmission: The vehicle by which the organism is transferred such as physical contact, inhalation, or injection. The most common vehicles are respiratory secretions spread by a cough, sneeze, or on the hands. A single sneeze can send thousands of virus particles into the air.
- Portal of Entry: The method by which the organism enters a new host, such as through mucous membranes or nonintact skin.
- Susceptible Host: The susceptible individual the organism has invaded.
For a pathogen to continue to exist, it must put itself in a position to be transmitted to a new host, leaving the infected host through a portal of exit. Similar to portals of entry, the most common portals of exit include the skin and the respiratory, urogenital, and gastrointestinal tracts. Coughing and sneezing can expel thousands of pathogens from the respiratory tract into the environment. Other pathogens are expelled through feces, urine, semen, and vaginal secretions. Pathogens that rely on insects for transmission exit the body in the blood extracted by a biting insect.
The pathogen enters a new individual via a portal of entry, such as mucous membranes or nonintact skin. If the individual has a weakened immune system or their natural defenses cannot fend off the pathogen, they become infected.
Infections can be stopped from spreading by interrupting this chain at any link. Chain links can be broken by disinfecting the environment, sterilizing medical instruments and equipment, covering coughs and sneezes, using good hand hygiene, implementing standard and transmission-based precautions, appropriately using personal protective equipment, encouraging patients to stay up-to-date on vaccines (including the flu shot), following safe injection practices, and promoting the optimal functioning of the natural immune system with good nutrition, rest, exercise, and stress management.
Disinfection and sterilization are used to kill microorganisms and remove harmful pathogens from the environment and equipment to decrease the chance of spreading infection. Disinfection is the removal of microorganisms. However, disinfection does not destroy all spores and viruses. Sterilization is a process used on equipment and the environment to destroy all pathogens, including spores and viruses. Sterilization methods include steam, boiling water, dry heat, radiation, and chemicals. Because of the harshness of these sterilization methods, skin can only be disinfected and not sterilized.[4]
To protect patients and health care workers from the spread of pathogens, the CDC has developed precautions to use during patient care that address portals of exit, methods of transmission, and portals of entry. These precautions include standard precautions and transmission-based precautions.
Standard precautions are used when caring for all patients to prevent healthcare-associated infections. According to the Centers for Disease Control and Prevention (CDC), standard precautions are the minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where health care is delivered. These precautions are based on the principle that all blood, body fluids (except sweat), nonintact skin, and mucous membranes may contain transmissible infectious agents. These standards reduce the risk of exposure for the health care worker and protect the patient from potential transmission of infectious organisms.
- Appropriate hand hygiene
- Use of personal protective equipment (e.g., gloves, gowns, masks, eyewear) whenever infectious material exposure may occur.
- Appropriate patient placement and care using transmission-based precautions when indicated.
- Respiratory hygiene/cough etiquette
- Proper handling and cleaning of environment, equipment, and devices
- Safe handling of laundry
- Sharps safety (i.e., engineering and work practice controls)
- Aseptic technique for invasive nursing procedures such as parenteral medication administration
In addition to standard precautions, transmission-based precautions are used for patients with documented or suspected infection of highly transmissible pathogens, such as C. difficile (C-diff), Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant enterococci (VRE), Respiratory Syncytial Virus (RSV), measles, and tuberculosis (TB). For patients with these types of pathogens, standard precautions are used along with specific transmission-based precautions.
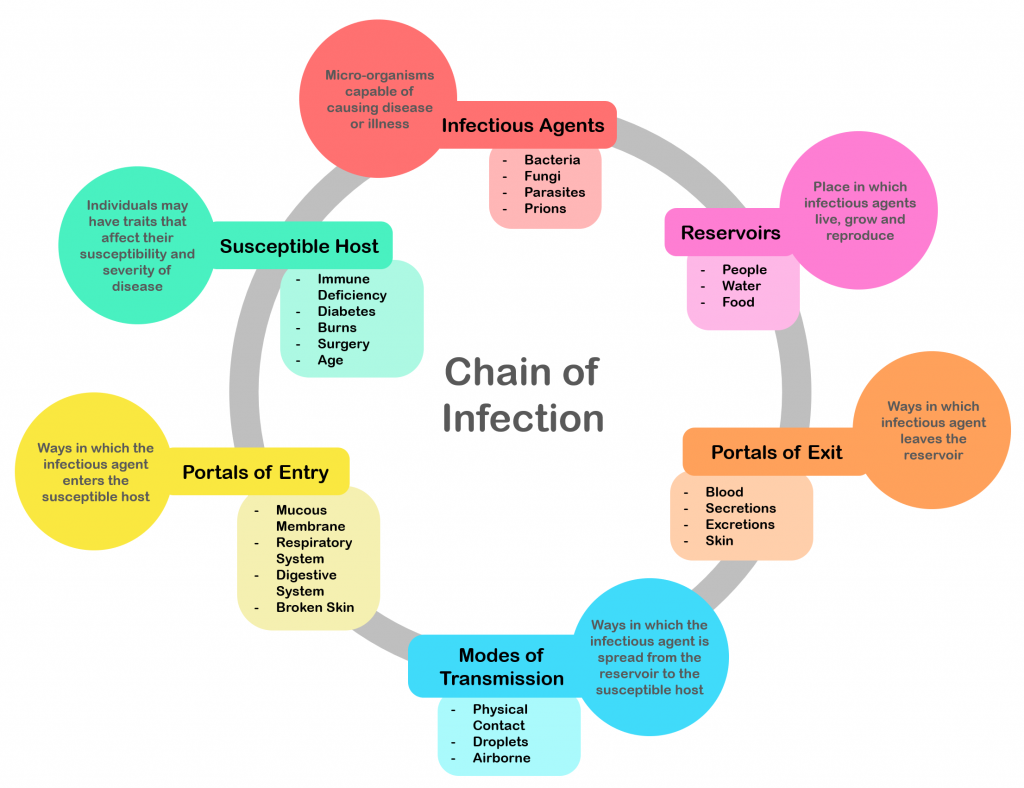
There are three categories of transmission-based precautions: contact precautions, droplet precautions, and airborne precautions. Transmission-based precautions are used when the route(s) of transmission of a specific disease are not completely interrupted using standard precautions alone.
Some diseases, such as tuberculosis, have multiple routes of transmission so more than one transmission-based precaution category must be implemented. See the table below outlining the categories of transmission precautions with associated PPE and other precautions.
Transmission-Based Precautions
Precaution | Implementation | PPE and Other Precautions |
Contact | Known or suspected infections with increased risk for contact transmission (e.g., draining wounds, fecal incontinence) or with epidemiologically important organisms, such as C-diff, MRSA, VRE, or RSV |
Note: Use only soap and water for hand hygiene in patients with C. difficile infection |
Enhanced barrier | Used during high-contact resident care activities for individuals colonized or infected with a multidrug-resistant organism (MDRO) as well as those at increased risk of MDRO acquisition |
|
Droplet | Known or suspected infection with pathogens transmitted by large respiratory droplets generated by coughing, sneezing, or talking, such as influenza, coronavirus, or pertussis |
|
Airborne | Known or suspected infection with pathogens transmitted by small respiratory droplets, such as measles, tuberculosis, and disseminated herpes zoster | Fit-tested N-95 respirator or PAPR
|
When possible, patients with transmission-based precautions should be placed in a single occupancy room with dedicated patient care equipment (e.g., blood pressure cuffs, stethoscope, and thermometer stay in the patient’s room). A card is posted outside the door alerting staff and visitors to required precautions before entering the room. See picture below for an example of signage used for a patient with contact precautions. Transport of the patient and unnecessary movement outside the patient room should be limited.
Contact Precautions Sign