Reproductive System
Reproductive System
Structures through which sperm pass to the exterior
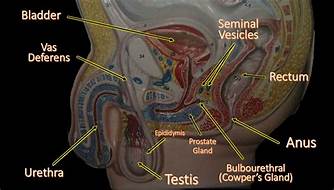
Testes - Sperm Production
1. Epididymis - Sperm storage and maturation. Sperm acquire motility and fertility.
2. Ductus (vas) deferens - Duct carrying sperm to urethra
3. Spermatic cord - Contains vas deferens, spermatic artery and vein, nerve cord to testes.
4. Seminal vesicle - Adds fructose rich fluid to sperm
5. Ejaculatory duct (in prostate) - Vas deferens and ducts from seminal vesicles form this
6. Urethra (in corpus spongiosum) - Passes trough penis (Dual role-reproductive and urinary)
7. External urinary meatus (in glans of penis)
a. Structure of Penis
Accessory Structures
1. Scrotum - Sac that contains the testes and keeps them at a lower temperature than inside body. Muscle can contract or relax to move the testes closer to or farther away from body for temperature regulation. Sperm do not develop properly at normal body temperature.
2. Seminal vesicles - Adds fructose rich fluid to sperm.
3. Prostate gland – Secretes alkaline fluid to add to ejaculate to neutralize acidity in vagina
4. Cowper’s glands – Also known as bulbourethral glands. The glands secrete a clear fluid rich in mucoproteins that help to lubricate the distal urethra and neutralize acidic urine which remains in the urethra.
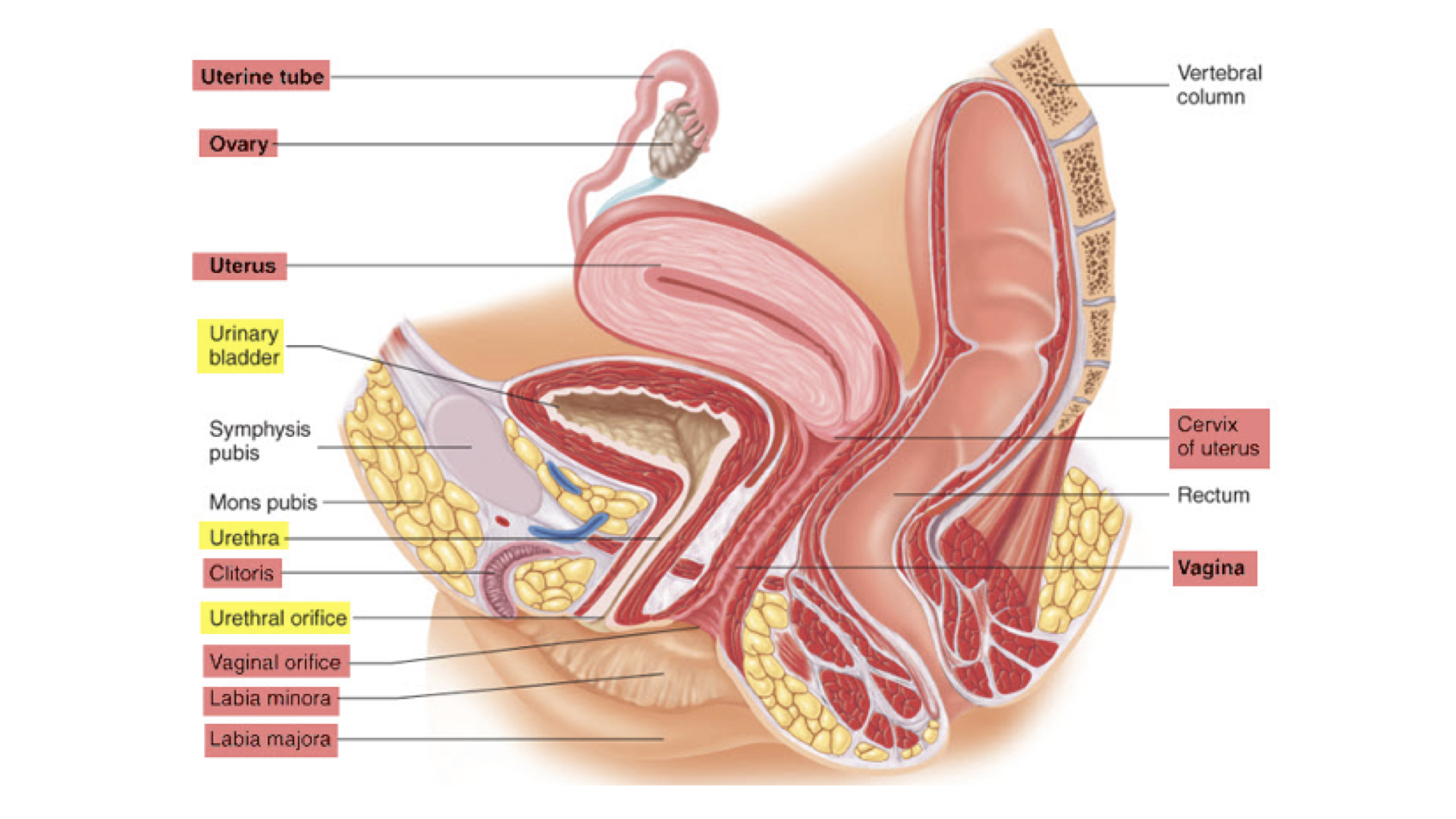
Structures mature ovum passes through to exterior
1. Ovaries - Starting with primordial follicle-->primary follicle-->secondary follicle-->mature ovum (Graafian follicle)-->ovulation. At this point the ovum has undergone only first meiotic division. Second meiotic division occurs in fallopian tube if fertilized. Corpus lute important for production of progesterone which maintains endometrium until placenta takes over that role.
2. Fallopian (uterine) tubes - Carry ovum to uterus where fertilization and first cell divisions occur. Passage of ovum takes about five days.
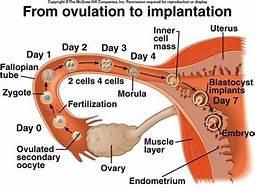
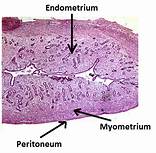
3. Uterus - This organ is where the fetus develops until birth. The uterus has three layers--endometrium, myometrium, and an outer perimetrium. It is held in place by several ligaments.

4. Vagina - Pathway from uterus to outside and for sperm entrance.
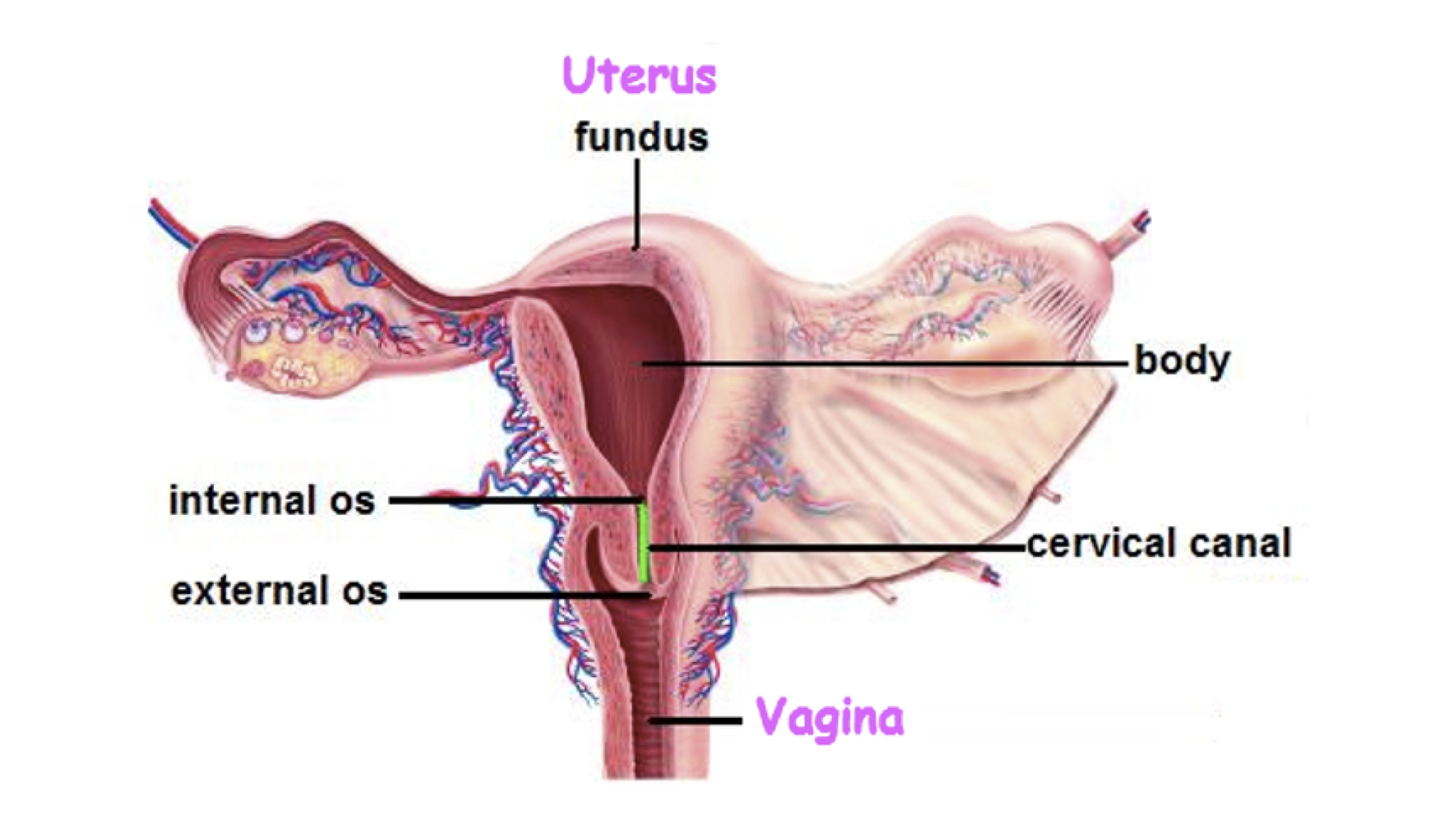
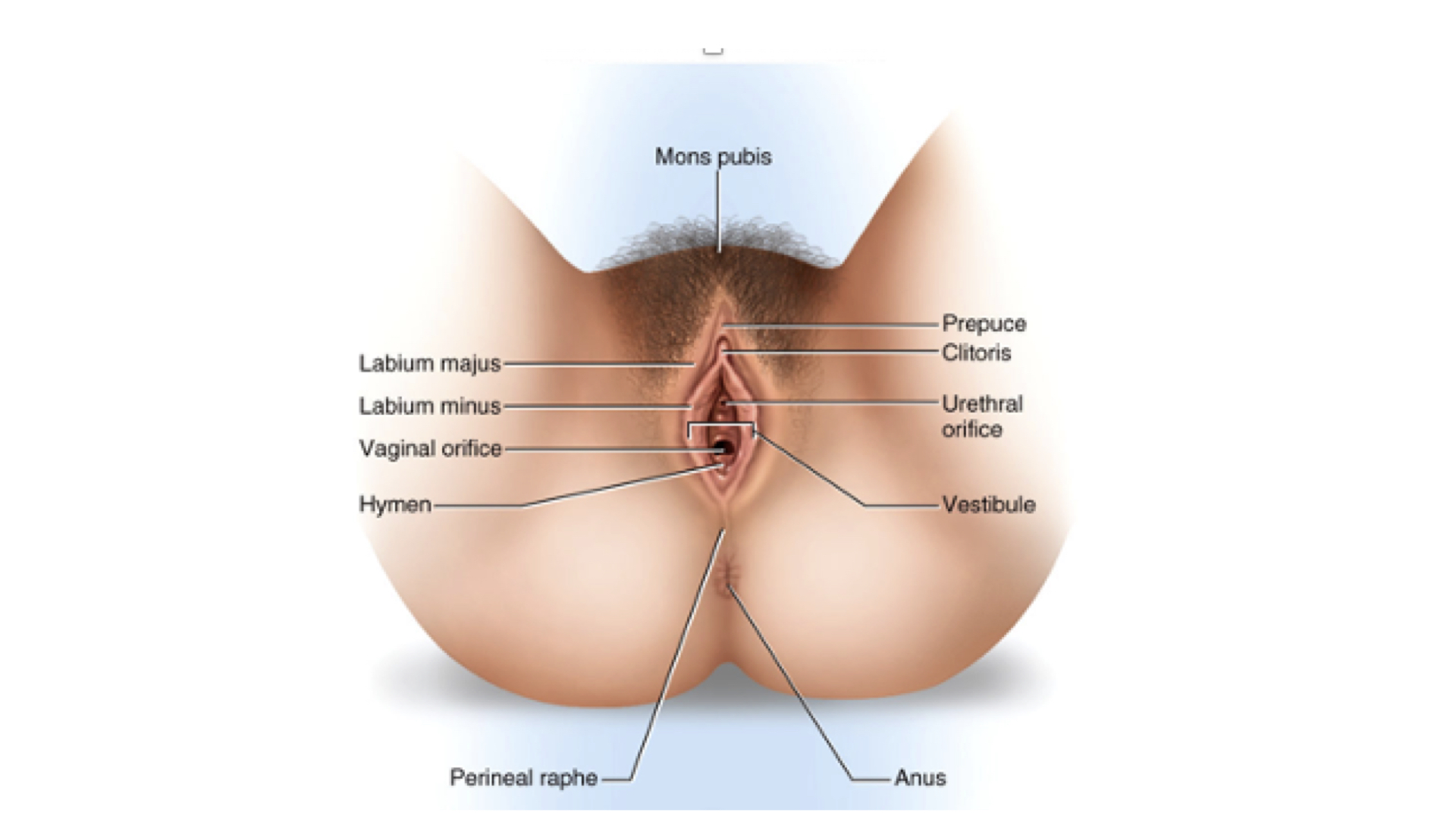
5. Vestibule - This is the part of the vulva between the labia minor into which both the urethra and vagina open.
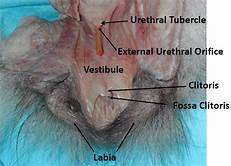
6. Structure of External Genitalia
a. Mons pubis
b. Labia majora
c. Labia minora
d. Clitoris
1. Corpora cavernosa with crus
2. Corpus spongiosum with glans
3. Prepuce = Foreskin
Accessory Structures
1. Skene’s glands - Located on the anterior wall of the vagina, around the lower end of the urethra. The ducts open on the anteriarbsidenofnthenvagina. Their function is not entirely known although the tissue is homologous to the prostate gland in males.
2. Bartholin’s glands - Located slightly posterior and to the left and right of the opening of the vagina. They secrete mucus to lubricate the vagina and are homologous to bulbourethral glands in males.
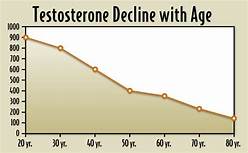
Puberty in males begins with an increase in Follicle Stimulating Hormone (FSH) which initiates spermatogenesis and Luteinizing Hormone (LH) which starts the increasing production of testosterone. While levels of these hormones decline with age, there is no cycling similar to the menstruai cycle in females.
In females, the same hormones begin to increase causing the changes indicated above. At some point in puberty menstruation begins. There are several hormones involved in regulating the cycle on a roughly monthly basis. At the start of the cycle FSH levels begin to increase. The rising estrprimordial follicles in the ovary to begin to develop culminating in one of them becoming a Graffian follicle. As the follicles develop, the ovary releases increasing levels of estrogen. The rise in estrogen causes the endometrium to thicken in preparation for a possible pregnancy. The rising FSH feedback to the hypothalamus causes a reduction in FSH. As estrogen levels continue to increase, LH levels spike, normally around the 14th day. Ovulation follows within 24 hours.
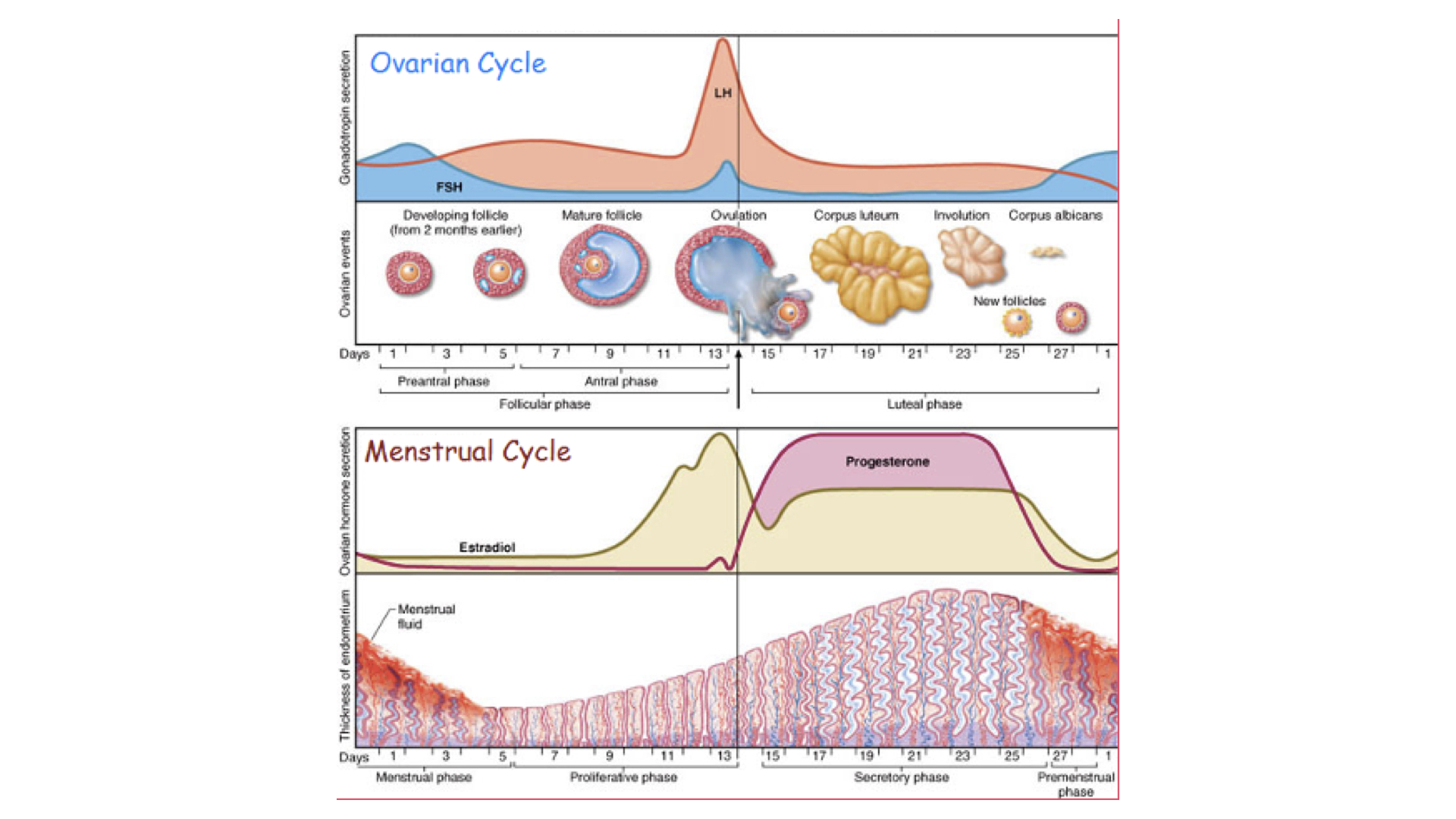
Following ovulation, LH drops rapidly and FSH also declines. Estrogen declines at the same time. the follicle becomes a corpus lute after ovulation produces large amounts of progesterone. The progesterone and estrogen continue to prepare the endometrium. If the ovum is not fertilized, the corpus luteum begins to stop producing progesterone which leads to loss of the endometrium in the menstrual flow.
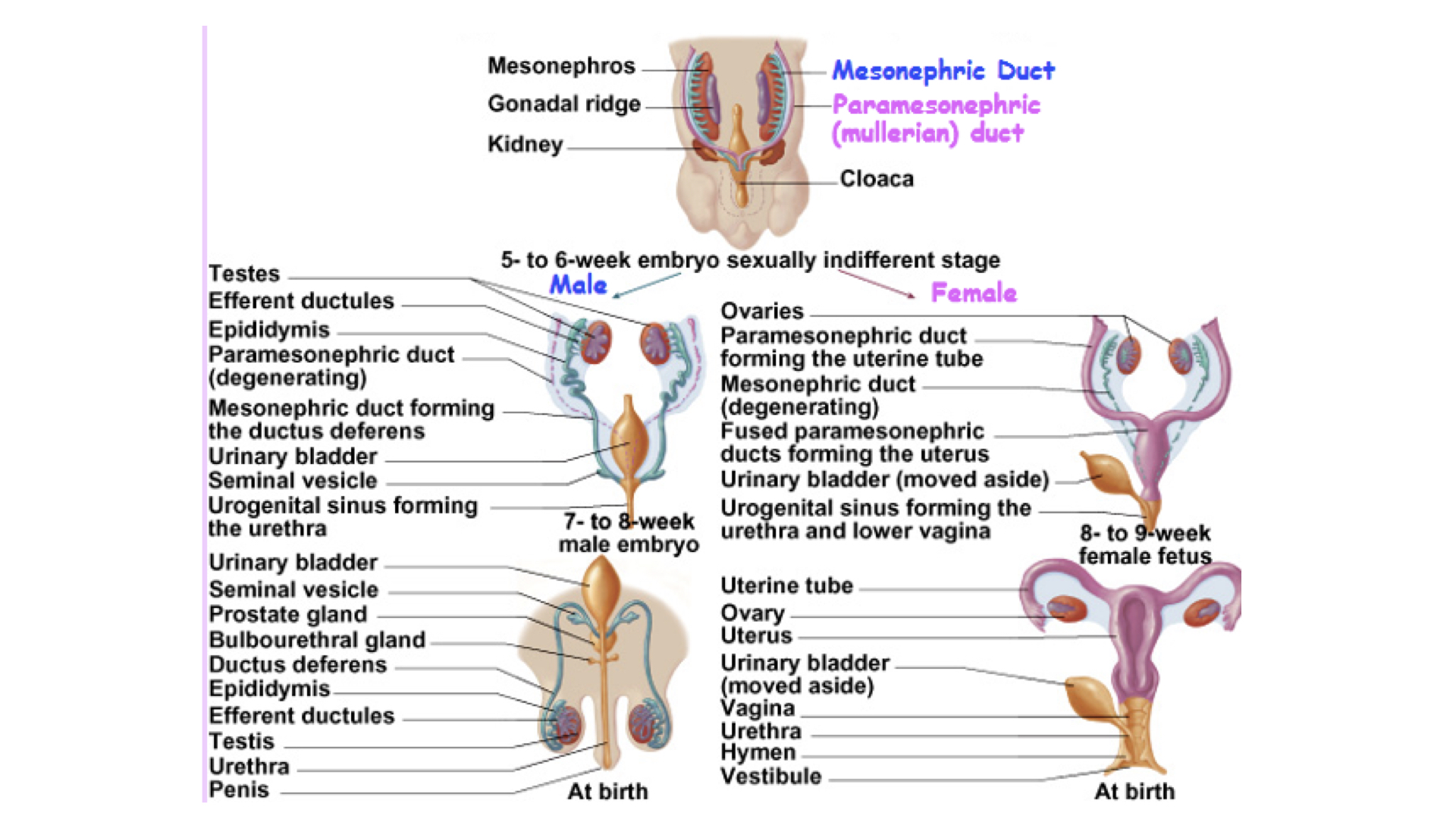
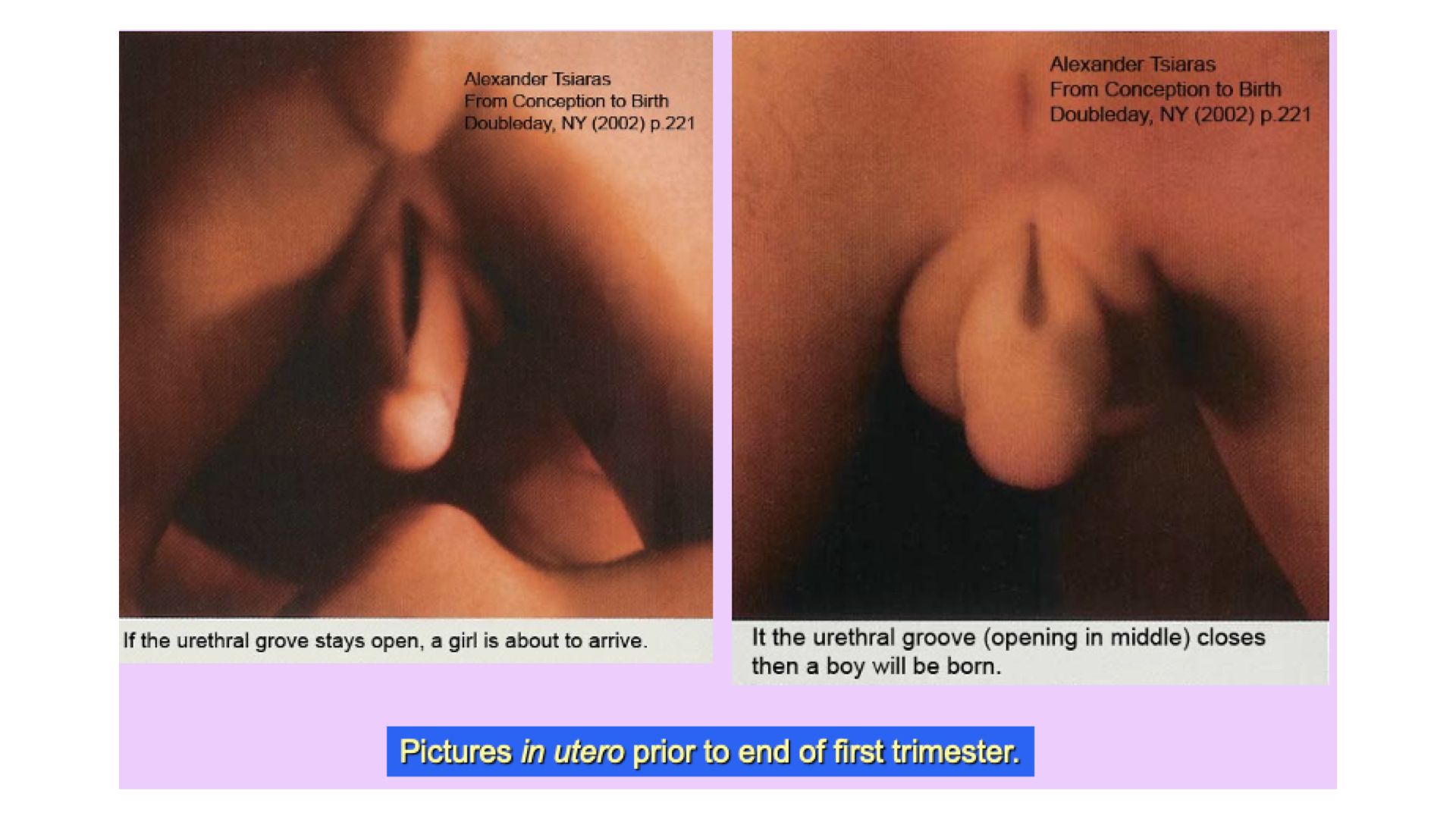
As the embryo begins to develop, male and female embryos are structurally identical. At five to six weeks two sets of ducts have developed--Mullerian and Wolffian. The Wolffian ducts are attached to to the metanephrose or primitive kidney. When testosterone begins to be secreted at about 7-8 weeks of development, this duct forms the epididymus, vas deferens, prostate, and the seminal vesicle. At this point the Mullerian ducts atrophy. The initiation of testosterone is directed by the SRY gene on the Y chromosome.
The Mullerian ducts are originally attached to the paramesonephric "kidney". In the absence of testosterone, the Mullerian ducts form the fallopian tubes, uterus, and the vagina. The Wolffian ducts atrophy in females.
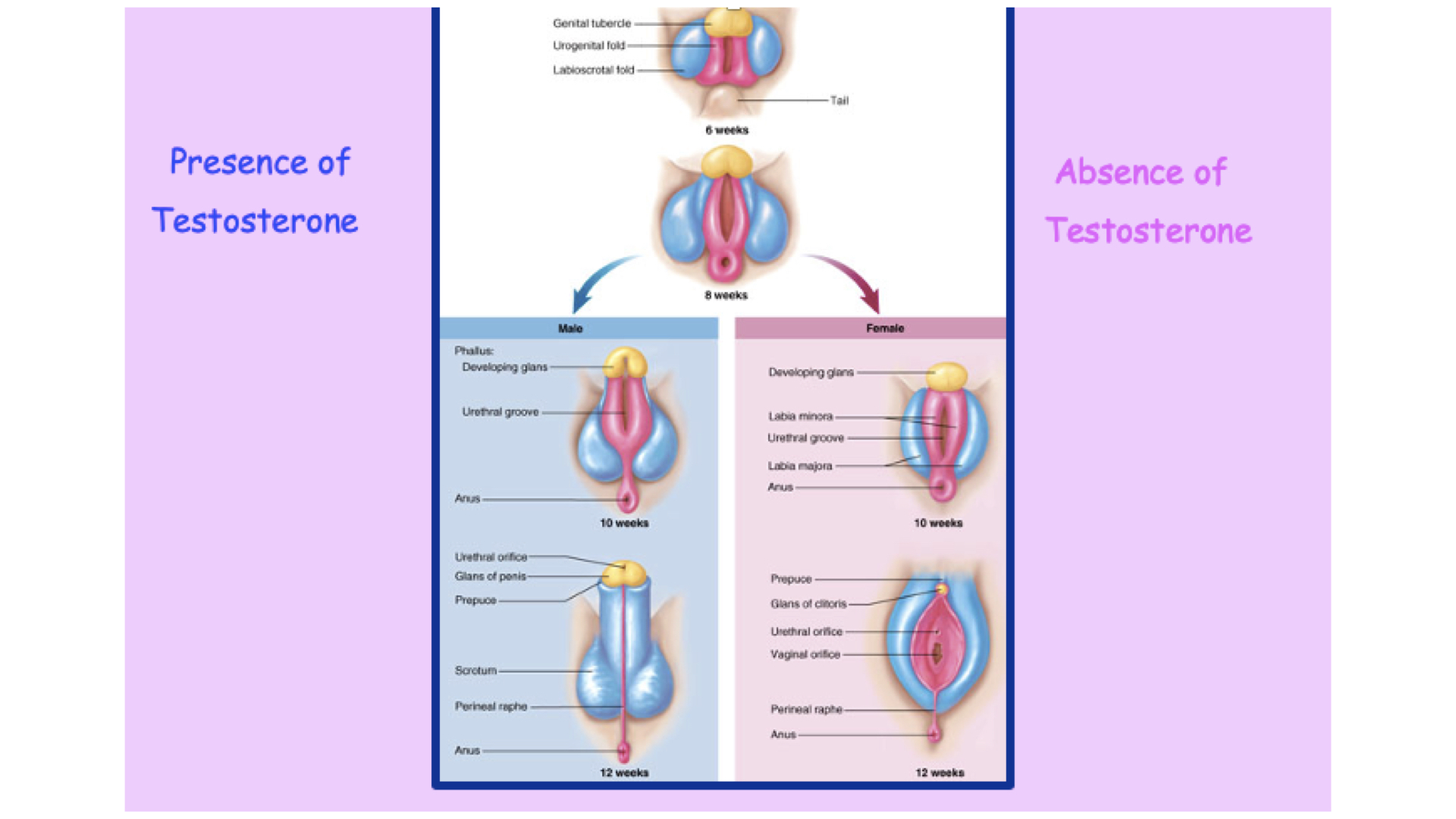
In cases where the embryo has an XY configuration but either the SRY gene in not finctional or, testosterone receptors are not functional, develop continues as female.
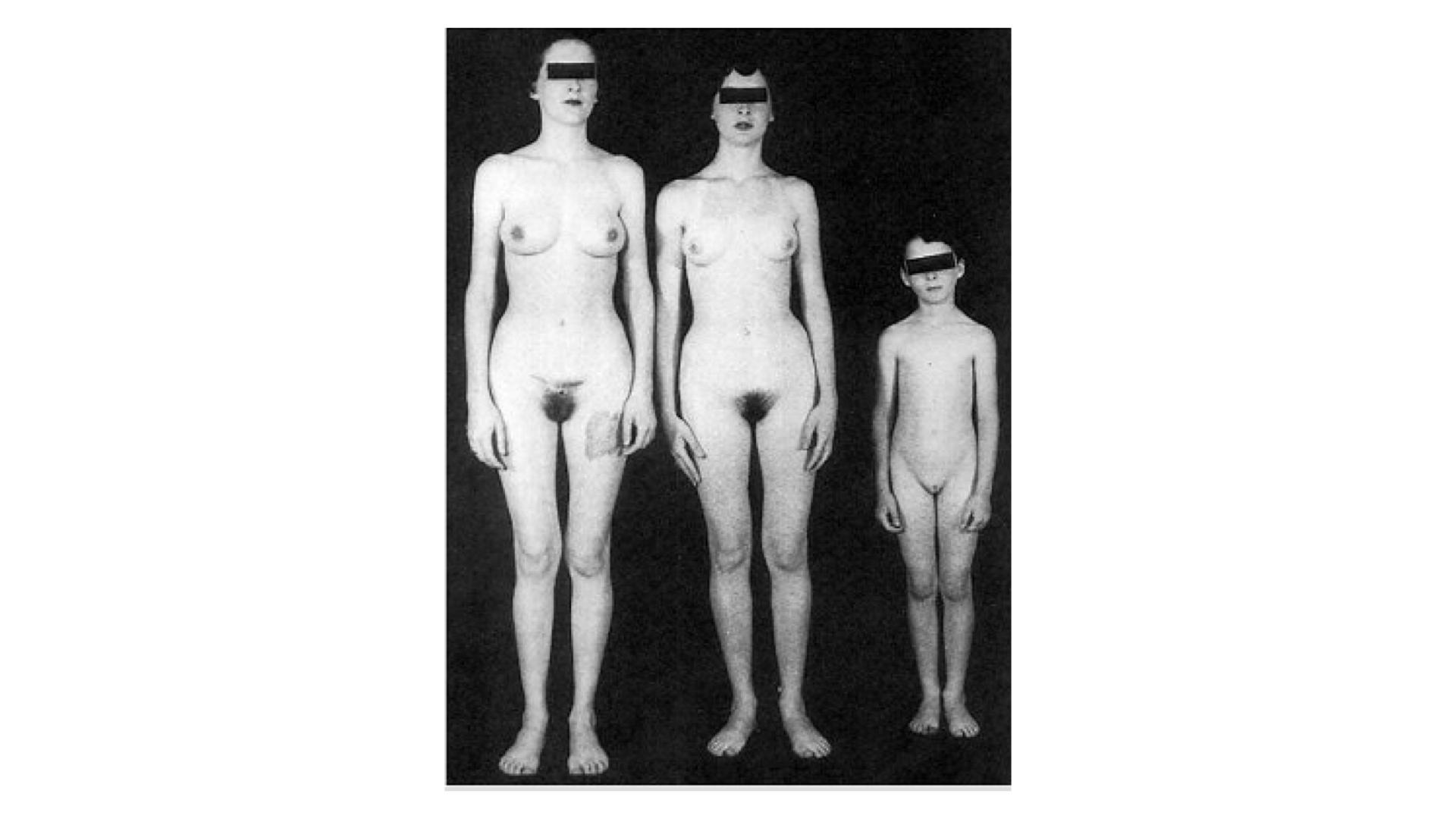 All Three are Genetically Male--XY
All Three are Genetically Male--XY
Many of the tissues in female and male reproductive systems are derived from the same embryonic tissues, simply shaped by developmental processes for different functions.
External
Male | Female |
Penis | Clitoris |
Corpus Spongiosum | Corpus Spongiosum |
Glans | Glans |
Corpora Cavernosa | Corpora Cavernosa |
Crus | Crus |
Foreskin | Prepuce (hood) |
Scrotum | Labia Majora |
Median Raphe | Labia Minora |
Mons Veneris | Mons Veneris |
Internal | |
Cowper’s Glands (Bulbourethral) | Bartholin’s Glands |
Prostate Gland | Skene’s Glands |
Utricle | Uterus |
Perineal Muscles | Perineal Muscles |
Bulbocavernosus (Surrounds Bulb of Penis, ejects semen | Bulbocavernosus (Surrounds Vaginal Opening) |
Ischiocavernosus (surrounds Crus) | Ischiocavernosus (surrounds Crus) |
Pubococcygeal | Pubococcygeal (Forms Orgasmic Platform) |
Tissues derived from the same embryonic structures in both sexes
1. Fertilization
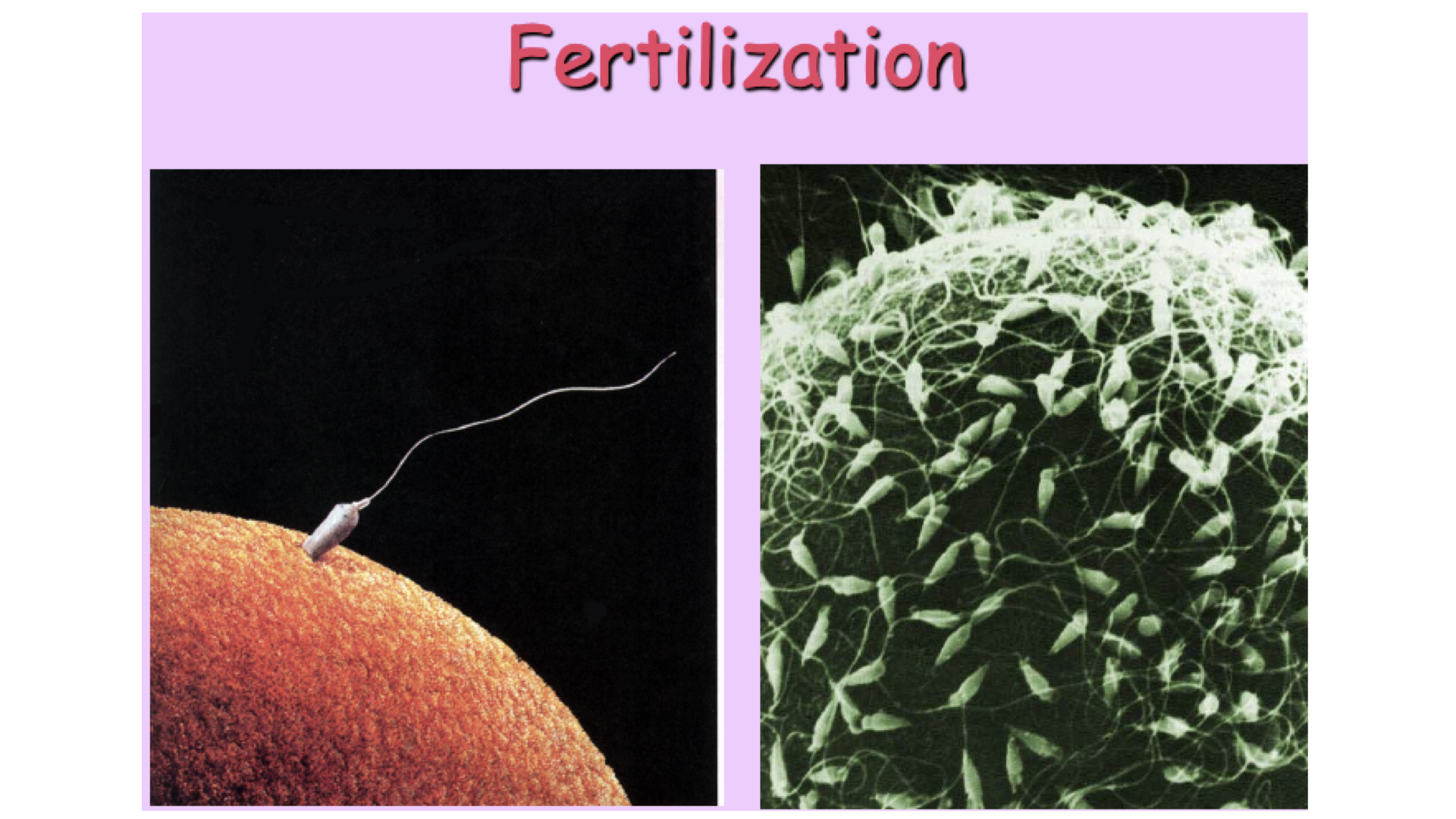
Fertilization occurs in the upper portion of the fallopian tube. The ovum is viable for 12 to 24 hours and the sperm are viable up to 5 days. After fertilization, the ovum begins cell division as it moves down the fallopian tube to implant in the endometrium.
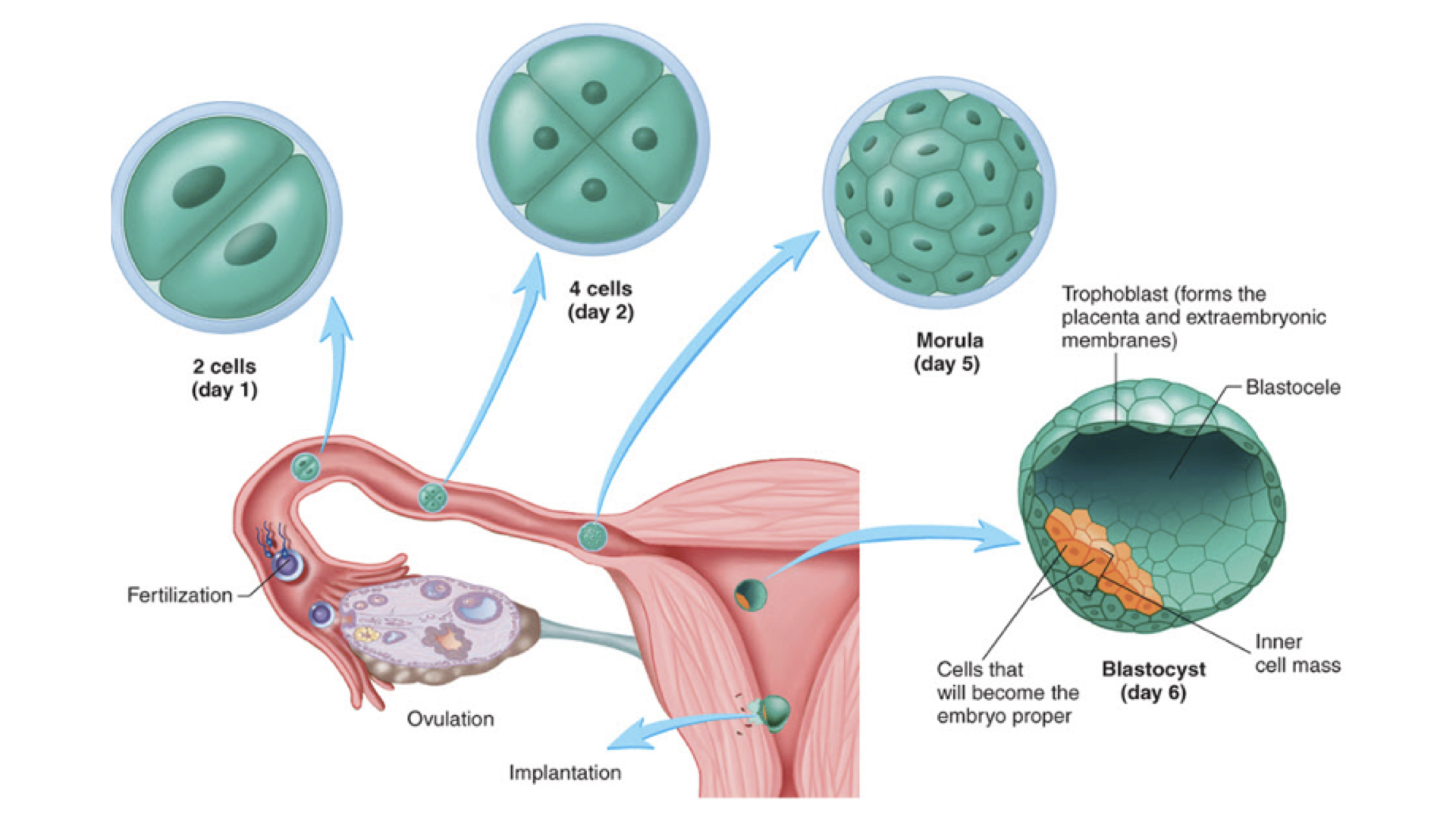
After the ovum begins to divide, it produces human chorionic gonadotropin (HCG). This maintains the corpus luteum and the progesterone it produces to maintain the endometrium. This is the hormone that causes a positive result in home pregnancy tests. High levels are produced; as a result, the kidneys filter out some of the hormone into the urine. Morning is best time to test because the hormone will have accumulated in the bladder overnight.
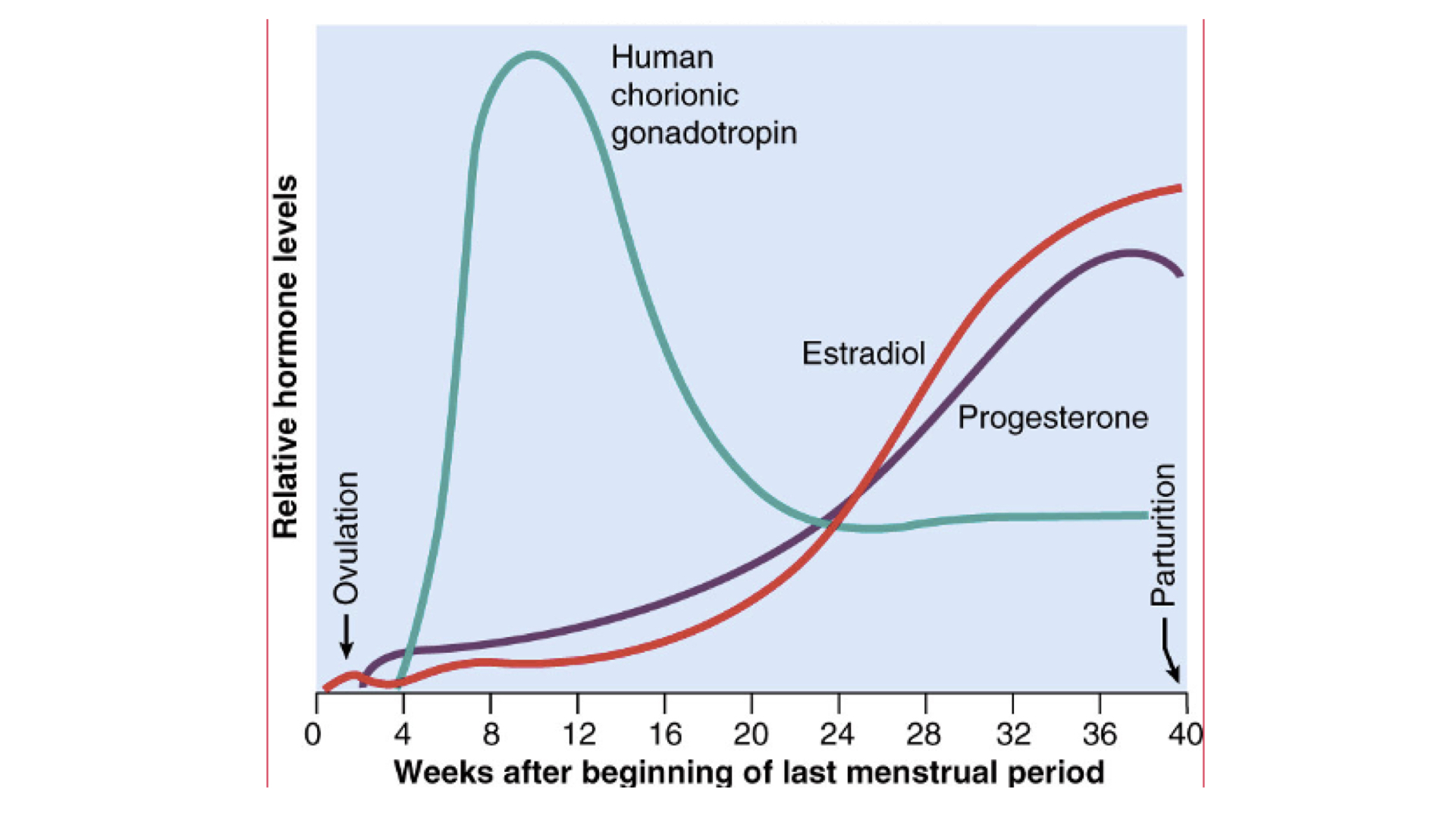
2. Gestation - 3 trimesters of 3 months (280 days total)
a. Embryonic Period (first trimester ) -
Fetal development in first trimester
b. Fetal Period ( second Trimester )
Fetal Development in second trimester
c. Fetal period (third trimester)
Fetal Development in third trimester
d. Parturition ( Birth ) - Oxytocin
As you get the close to delivery, the fetus drops down in the uterus and hopefully ends up head and shoulders down. There are stretch receptors in the lower part of the uterus. eventually there is enough pressure to feedback to the brain and the posterior pituitary gland releases oxytocin. one of the effects of that hormone is to cause contraction of smooth muscles, like those in the myometrium. there are often a few false starts but eventually the pressure on the receptors increases contractions. Contractions cause increased pressure on the stretch receptors. Contractions continue to get stronger in this positive feedback loop. Once the head and shoulders pass through the cervix, much of the pressure is relieved. Contractions continue to deliver the placenta, usually in 10-30 minutes.
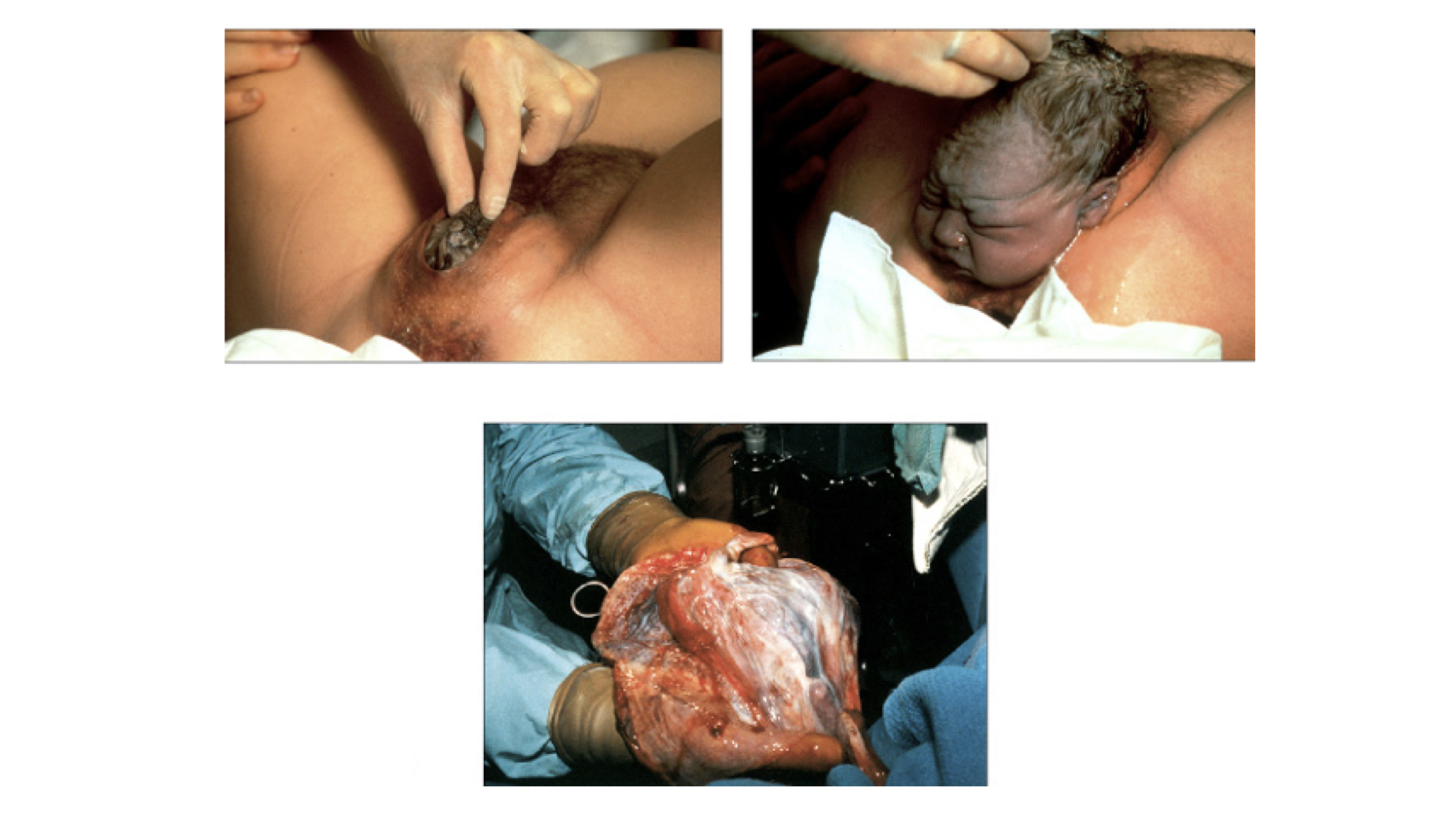
If the fetus is in the wrong position, too large, or if labor has been too long without birth, a Cesarean section may be required.
e. Prenatal Diagnostic Techniques
1. Amniocentesis - In this process the amniotic fluid is sampled. There is some risk because a needle must be inserted through the membranes into the amniotic fluid.
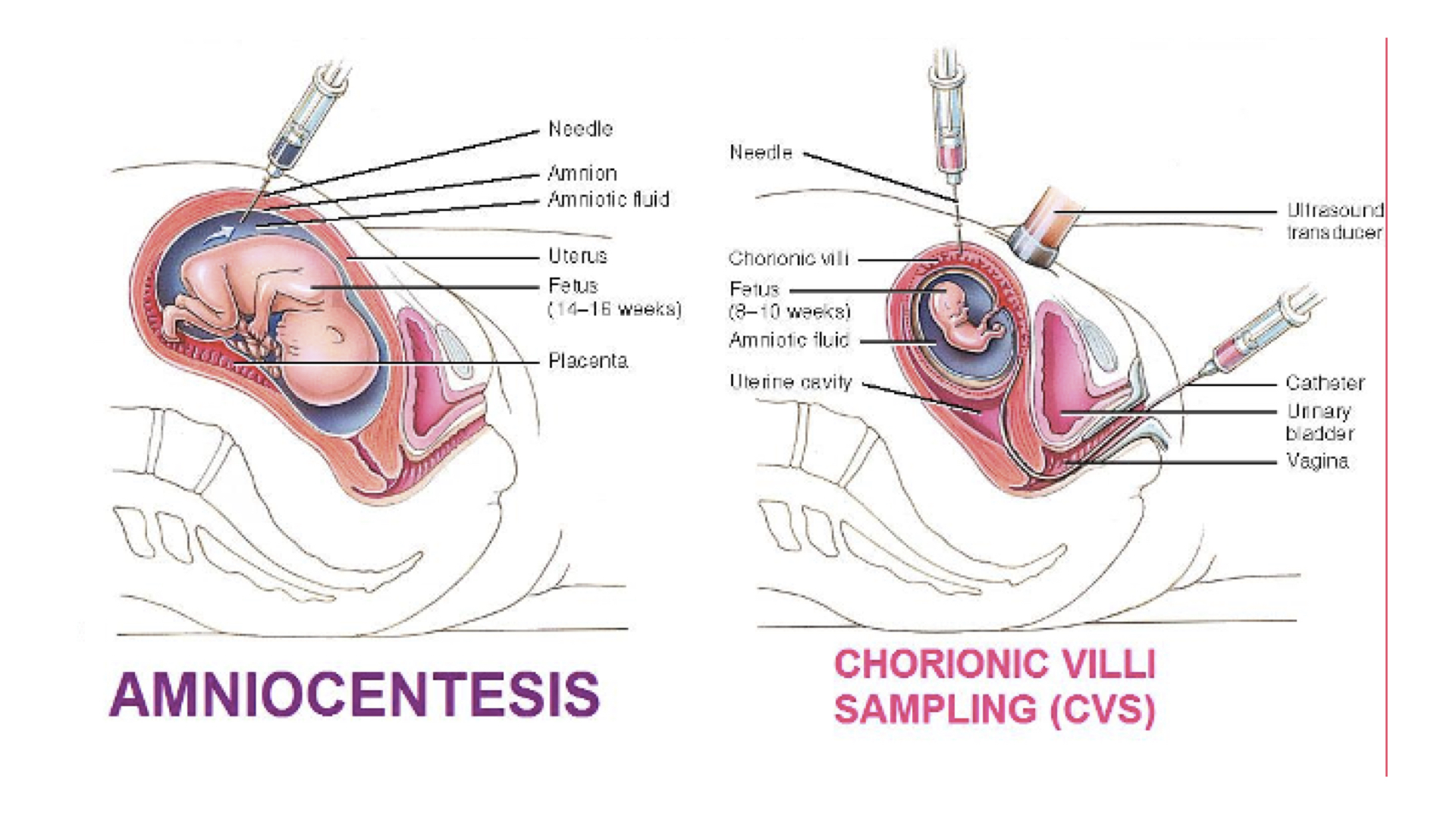
2. Chorionic Villi Sampling - This process has less risk as the needle only needs to go into the amnion to take sample and not all the way through into the fluid.
In both cases, the cells obtained are fetal cells.