Structure and Function of the Urinary System
Structure and Function of the Urinary System
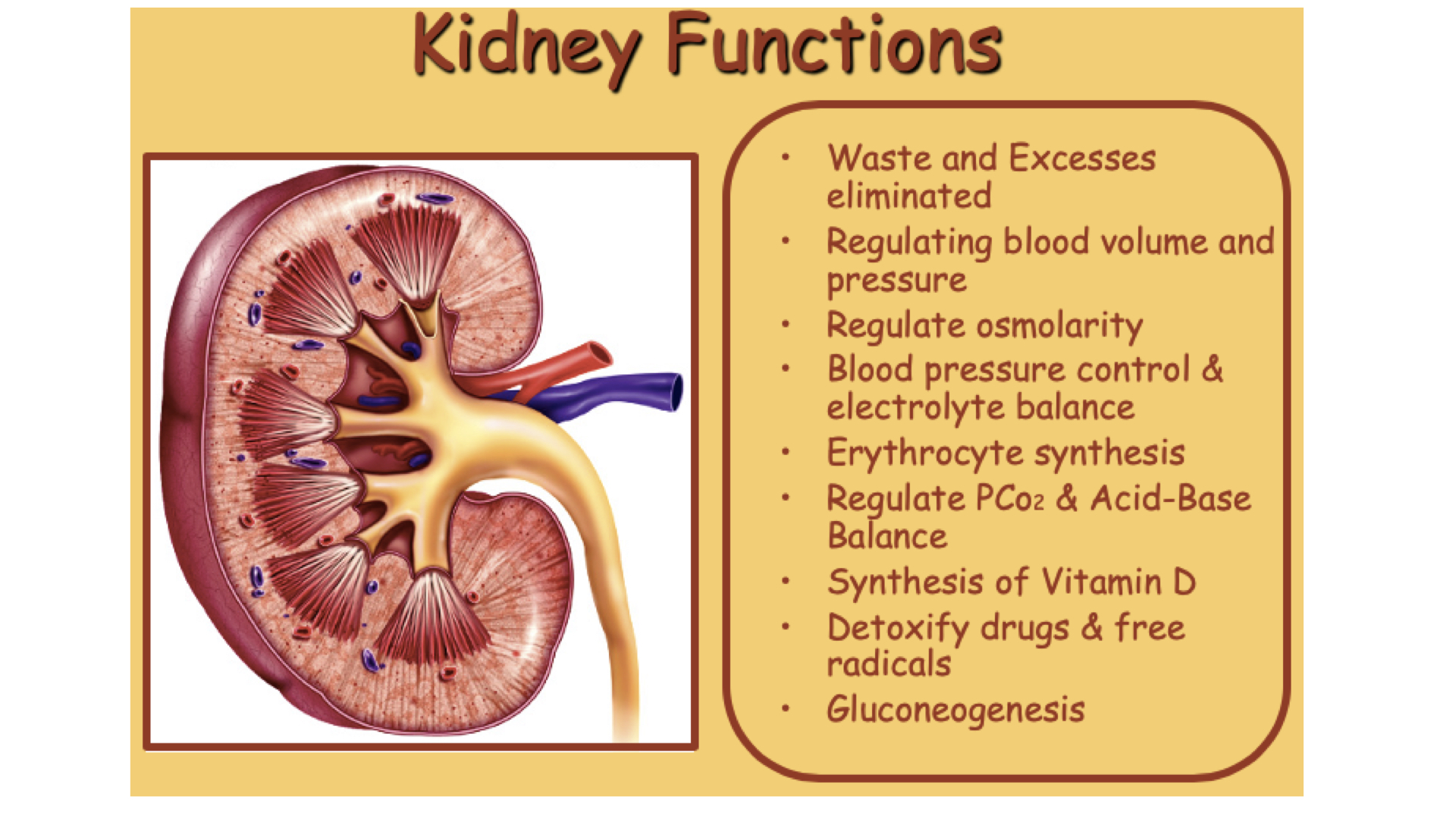
The urinary system has many functions. Most people intuitively know that it is an excretory system. However it is not the only system that does that. The integumentary, digestive and respiratory systems also excrete materials as well and you should review those systems even though the primary topic of this Chapter is the urinary system.
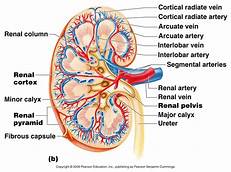
1. Structure of a kidney
- Hilus - point of entry for renal artery, and exit for renal vein and ureter.
- The ureter expands into the renal pelvis, which in turn is divided into major and minor calyces.
- Renal papillae project into the renal sinus.
- Kidney tissue is divided into a renal medulla and renal cortex.
2. Location of the kidneys
- The kidneys are on either side of the vertebral column, high on the posterior wall of the abdominal cavity
- They are positioned behind the parietal peritoneum and held in place by adipose and connective tissue, abdominal organs.
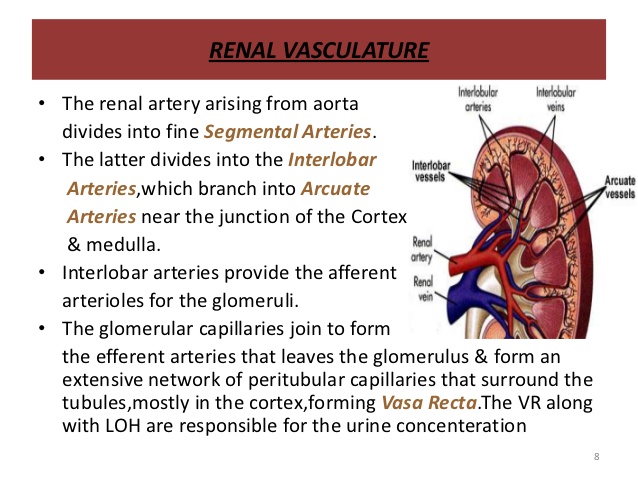
3. Renal blood vessels
- Arterial blood flows through the renal artery, interlobar arteries, arcuate arteries, interlobular arteries, and afferent arterioles.
- Venous blood returns through a series of vessels that correspond to those of the arterial pathways.
- Blood supply of a nephron
1. The glomerular capillary receives blood from the afferent arteriole and passes it to the efferent arteriole
2. The efferent arteriole gives rise to the peritubular capillary system that surrounds the renal tubule.
3. Capillary loops, called vasa recta, dip down into the medulla.
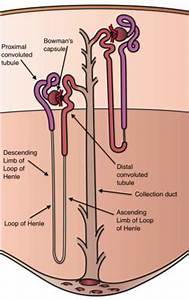
1. Structure of the nephron
- The nephron is the functional unit of the kidney.
- It consists of a renal corpuscle and a renal tubule.
1. The corpuscle consists of a glomerulus and a Bowman's capsule
a. produces filtrate - basically a protein-free solution
2. Portions of the renal tubule include the proximal convoluted tubule, the loop of Henle (ascending and descending limbs), the distal convoluted tubule, and the collecting duct.
- The collecting duct empties into the minor calyx of the renal pelvis.
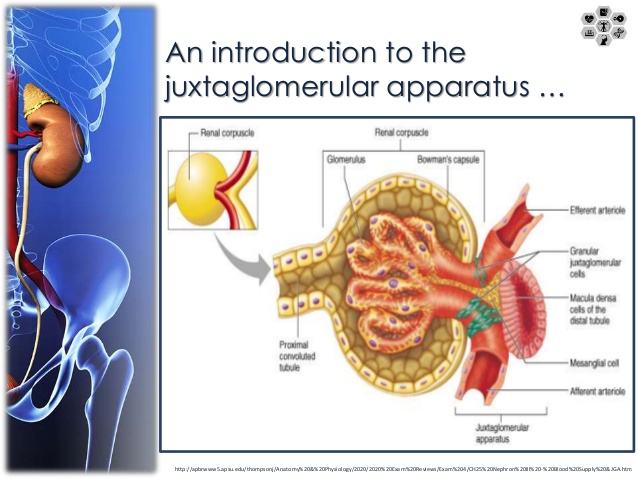
2. Juxtaglomerular apparatus
- The juxtaglomerular apparatus is located at the point of contact between the distal convoluted tubule and the afferent and efferent arterioles.
- It consists of the macula densa and the juxtaglomular cells
- Releases renin into the blood
Nephrons function to remove wastes from blood and to regulate water and electrolyte concentrationsUrine is the end product of these functions, which involve filtration, reabsorption, and secretion of substances from renal tubules.
Glomerular filtration
- Urine formation begins when water and dissolved materials are forced out of the glomerular capillary
- The glomerular capillaries are much more permeable than the capillaries in other tissues.
- Fenestrated - containing pores
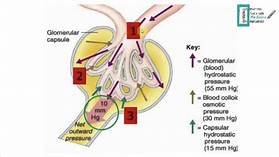
Filtration pressure
- Filtration is due mainly to hydrostatic pressure inside the glomerular capillaries.
- Filtration pressure is the net force acting to move material out of the glomerulus and into the Bowman's capsule.
Glomerular Filtration Rate (GFR)
- The rate of filtration varies with the filtration pressure
- Filtration pressure changes with the diameters of the afferent and efferent arterioles
- Filtration rate varies with the rate of blood flow through the glomerulus.
- The kidneys produce about 125 ml of glomerular fluid per minute, most of which is reabsorbed.
- The volume of filtrate varies with the surface area of the glomerular capillary.
Regulation of glomerular filtration rate
- When the filtration rate decreases, the macula densa dilate the afferent arteriole, which increases the blood flow through the glomerulus and increases the filtration rate.
1. Renin®anginotensinogen ®angiotensin II
- Autoregulation is the ability of an organ or tissue to maintain a constant blood flow when the arterial blood pressure is changing
- Atrial natriuretic peptide (ANP) - increase GFR
The embedded video gives an overview of all three parts of urine formation. More information below.
Tubular reabsorption
- Substances are selectively reabsorbed from the glomerular filtrate.
- The peritubular capillary is adapted for reabsorption.
1. It carries low-pressure blood.
2. It is very permeable.
- Most reabsorption occurs in the proximal tubule where the epithelial cells possess microvilli.
- Various substances are reabsorbed in particular segments of the renal tubule by different modes of transport.
1. Sodium, glucose and amino acids are reabsorbed by active transport.
2. Water is reabsorbed by osmosis
3. Chloride ions are reabsorbed by diffusion.
- Active transport mechanisms have limited transport capacities.
- If the concentration of a substance in the filtrate exceeds its renal plasma threshold, the excess is excreted in the urine.
- Substances that remain in the filtrate are concentrated as water is reabsorbed.
Regulation of urine concentration and volume
- Most sodium is reabsorbed before urine is excreted.
- Sodium is concentrated in the renal medulla by the countercurrent mechanism.
1. Water leaves the descending limb by osmosis, and NaCl enters this limb by diffusion.
2. Tubular fluid in the descending limb becomes hypertonic as it loses water and gains NaCl.
3. Chloride ions are actively pumped out in the ascending limb and sodium ions follow them passively. Urea, uric acid, creatinine remain in the tube.
4. Tubular fluid in the ascending limb becomes hypotonic as it loses solutes.
- The vasa recta countercurrent mechanism helps to maintain the NaCI concentration in the medulla.
- The distal tubule and collecting duct are impermeable to water , so water is excreted in the urine
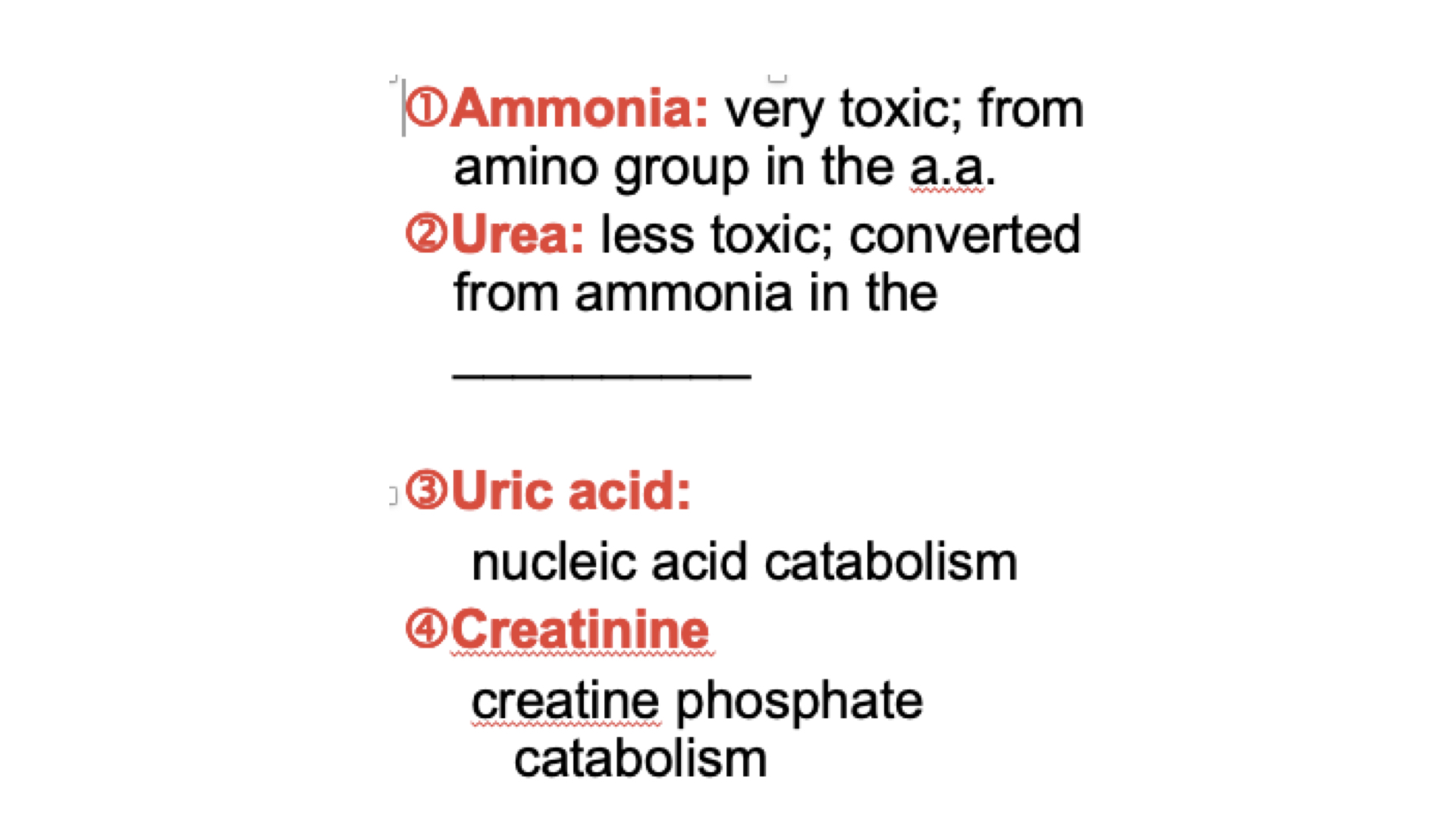
Waste Products Excreted
- Urea is a by-product of amino acid metabolism
1. It is reabsorbed passively by diffusion
2. About 5O% is excreted in urine.
3. A countercurrent mechanism helps in the excretion of urea.
- Uric acid results from the breakdown and recycling of RNA
1. Most is reabsorbed by active transport.
2. Some is secreted into the renal tubule.
- Creatinine generated by the breakdown of creatine phosphate
1. high energy compound used in skeletal muscle
- Tubular secretion
1. Tubular secretion is the process by which certain substances are transported from the plasma to the tubular fluid.
2. Some substances are secreted actively
a. These include various organic compounds and hydrogen ions.
b. Hydrogen ions are secreted by the proximal and distal segments of the renal tubule.
- Potassium ions are secreted passively in the distal segment and collecting duct where they are attracted by the negative charge that develops in the lumen of the tubule.
- Composition of urine
1. Urine is about 95% water and it usually contains urea, uric acid, and creatinine.
2. it may contain a trace of amino acids and varying amounts of electrolytes, depending upon the dietary intake'.
3. The volume of urine varies, with the fluid intake and with environmental factors.
The ureter
- The ureter is a tubular organ that extends from the kidney to the urinary bladder.
- The wall has mucous, muscular and fibrous layers.
- Peristaltic waves in the ureter force urine to the bladder.
- Obstruction in the ureter stimulates strong peristaltic waves and a reflex that causes the kidney to decrease urine production.
The urinary bladder
- The urinary bladder is a distensible organ that stores urine and forces it into the urethra.
- The openings for the ureters and urethra are located at the three angles of the trigone
- Muscle fibers in the wall form the detrusor muscle.
Micturition- the process by which urine is expelled.
- It involves contraction of the detrusor muscle and relaxation of the external urethral sphincter
- Micturition reflex
1. stretch receptors in the bladder are stimulated by distension.
2. reflex center in the sacral spinal cord sends parasympathetic motor impulses to the detrusor muscle
3. Urination can be controlled by means of the voluntary external urethral sphincter and nerve centers in the brain that can inhibit the micturition reflex.
4. When the decision to urinate is made the external urethral sphincter is allowed to relax and nerve centers in the brain act to facilitate the micturition reflex.
The urethra
- The urethra conveys urine from the bladder to the outside
- in females it empties between the labia minora.
- In males it conveys products of reproductive organs as well as urine
1. There are three portions of the male urethra: prostatic, membranous, and penile,
2. It empties at the tip of the penis.