How O2/CO2 Exchange Occurs in Lungs
How O2/CO2 Exchange Occurs in Lungs
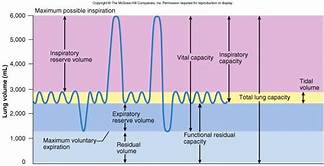
1. Tidal volume (VT)- average amount of air expired after a normal inspiration
2. Inspiratory reserve volume (IRV) - amount of air that can be forcibly inspired after normal inspirations
3. Expiratory reserve volume (ERV) - amount of air that can be forcibly expired after normal expirations
4. Vital capacity (VC) - maximum amount of air that can be moved in and out in a single respiratory cycle
5. Residual volume (RV) - amount of air that can not be forcibly expired
6. Minimal volume (MV) - amount of air that remains in the lungs after a pneumothorax and the lungs collapse
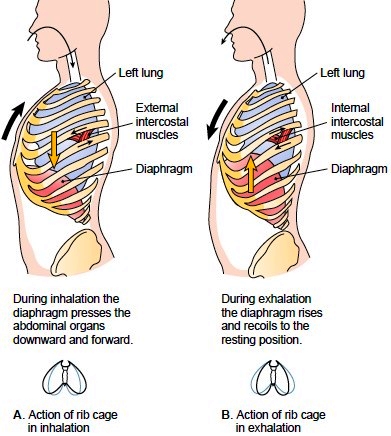
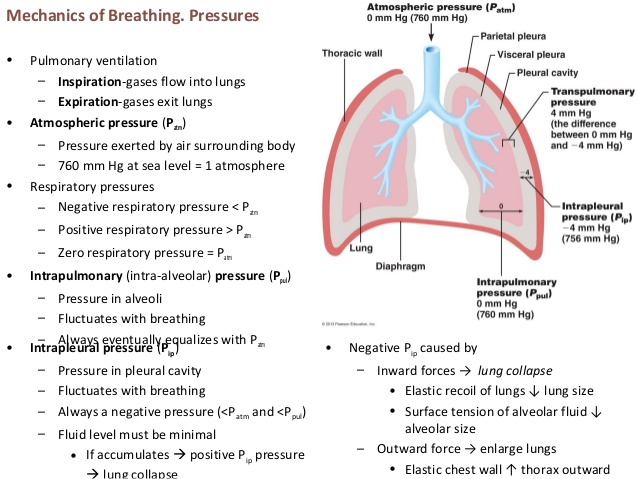
a. Ventilation - physical movement of air into and out of the lungs - to maintain adequate alveolar ventilation
b. inspiration - air pressure within the lungs falls below atmospheric pressure
c. expiration - air pressure within the lungs is above atmospheric pressure
d. Muscles of breathing
1. external intercostal - elevate the rib cage
2. internal intercostal - work during heavy breathing
3. diaphragm - relaxed shape is a dome during contraction it flattens and increases
the volume of the thoracic cavity
4. abdominals - assist in forced exhalation
Compliance - indicates the expandability of the lungs
Depends upon 2 factors
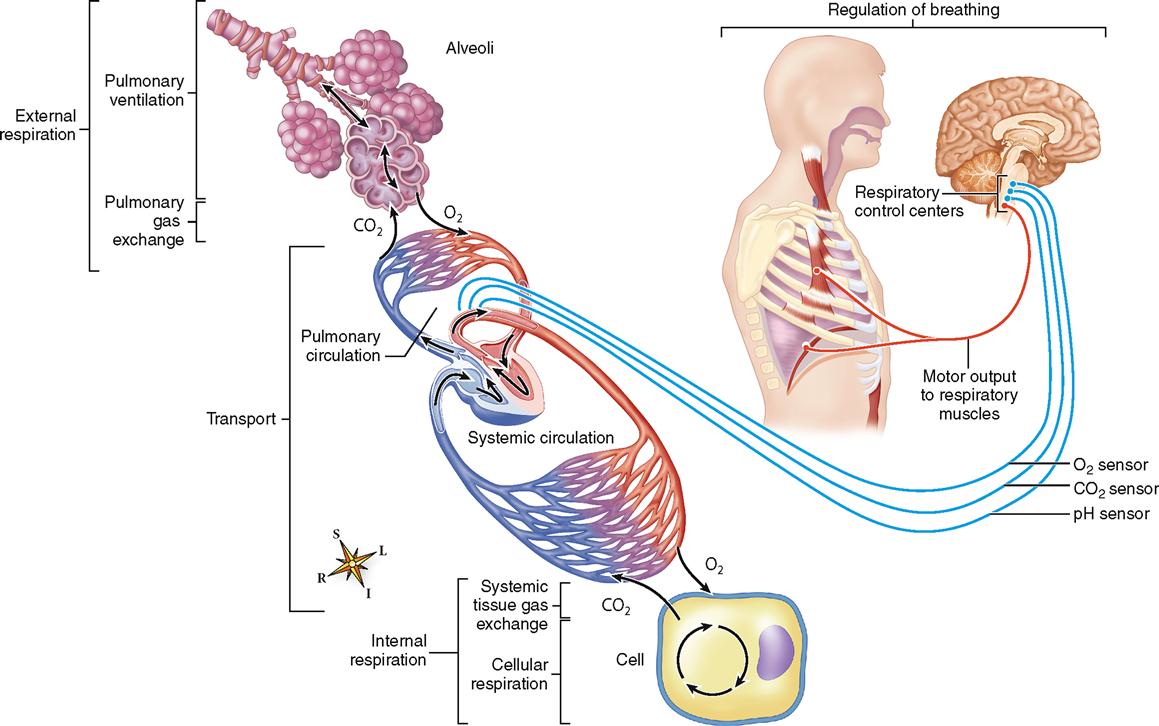
a. The partial pressure of the gases involved. Imagine a jar with a number of items in it-->marbles, sand, gravel, and water. If you weighed it, the total weight would be made up of the weight of each those. Marbles are then a partial weight, sand is a partial weight, gravel would be another partial weight, and water a partial weight. In the same way, the pressure of a gas is made up of of the partial pressures do to each of the components. Air is made up primarily of nitrogen, oxygen, carbon dioxide and a mix of other minor components.
b. The diffusion of a gas into a liquid. When inhale and air enters the lungs, the partial pressure due to oxygen in the air is higher than the pressure of oxygen in the blood returning in veins from the tissues which get to the lungs through the pulmonary arteries. As a result, oxygen diffuses from the lung not the capillaries of the alveoli in the lungs. For carbon dioxide, the reverse will be true and it will diffuse from the capillaries to the lungs. When you exhale, carbon dioxide returns to the atmosphere.
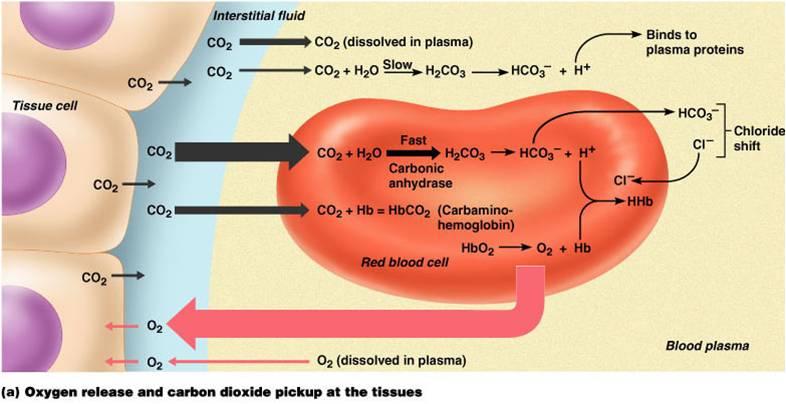
The blood stores and carries the respiratory gases between the alveolar capillaries and the capillary beds in other tissues. Normally about 98.5% of the oxygen is transported attached to hemoglobin in the red blood cells. A small amount is dissolved in the plasma.
Transport of oxygen in the Blood
When the blood returns to the heart and then is moved through the aorta to all parts of the body, the partial pressure of oxygen in the capillaries will be higher than in the tissues. Oxygen will diffuse into the tissues and carbon dioxide from the tissues into the blood to be carried to the lungs. About 5% is transported in the plasma, about 10% attached to hemoglobin, and the rest as bicarbonate ions in the blood:
CO2+H2O⟷H2CO3(carbonic acid)⟷HCO3+H+(bicarbonate)
Transport of Carbon Dioxide in the Blood
Gas exchange at the tissue level works on the same principle as in the lungs. The difference is that partial pressure of oxygen in the blood is higher than in the interstitial fluids-->so oxygen leaves hemoglobin and diffuses into the fluids. Carbon dioxide does the reverse.
Three factors that affect the release of oxygen from the oxyhemoglobin molecule:
a. P O2 - low pressure = greater release
b. pH - when pH declines hemoglobin releases more O2
c. Temperature - increase
Respiration is controlled by both neural centers and by chemical changes in homeostasis.
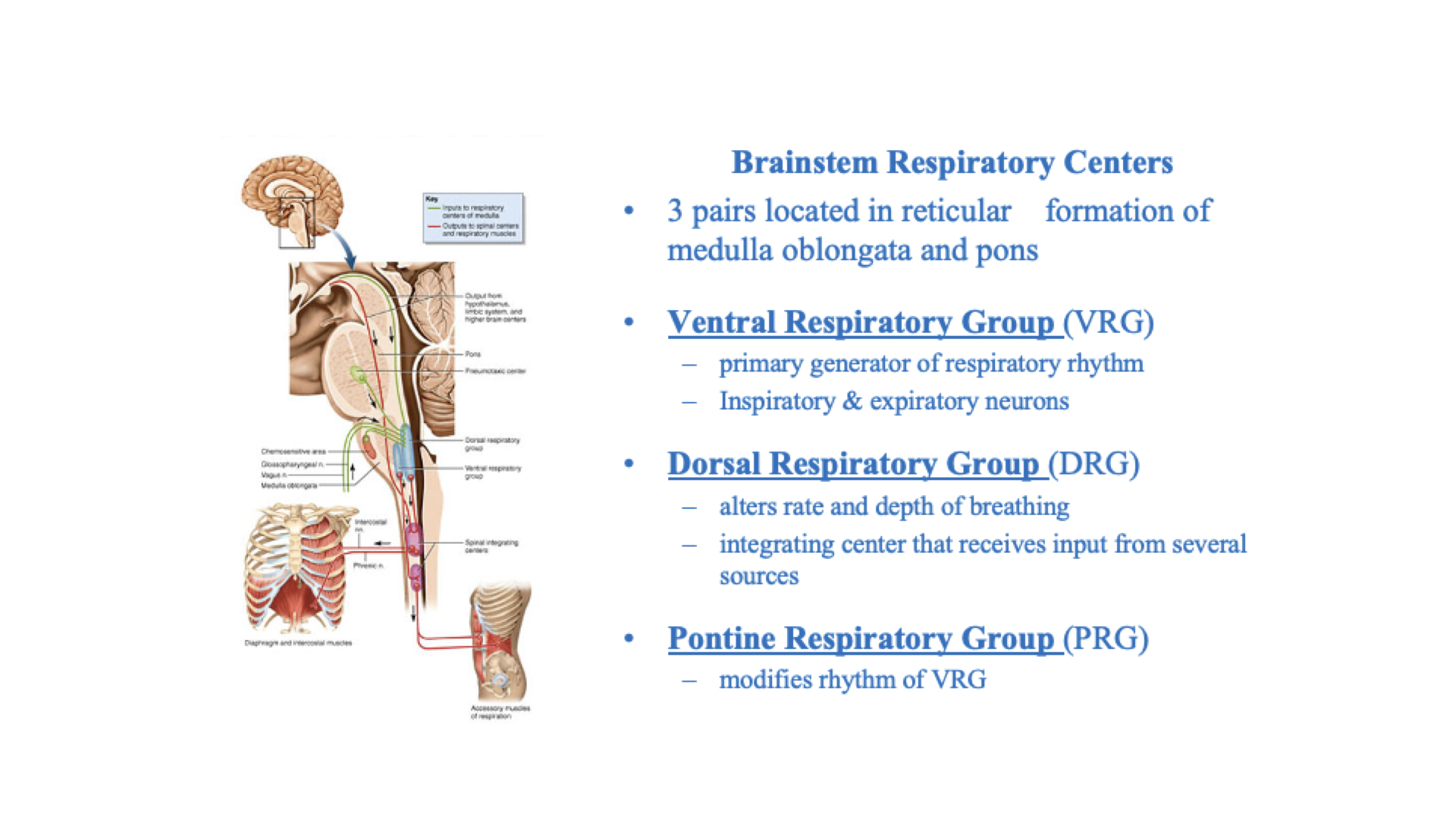
There are three important chemical stimuli of breathing.
- pH is the most potent stimulation. Acidosis and Alkilosis.
- Carbon dioxide is the next most important.
- Oxygen is the least important
Respiratory Adaptations to Exercise
- Athletic training
Vital capacity increases slightly; residual volume decreases slightly
At maximal exercise, tidal volume and minute ventilation increases
Gas exchange between alveoli and blood increases at maximal exercise
Alveolar ventilation increases
Increased cardiovascular efficiency leads to greater blood flow through the lungs
2. Ventilation increases abruptly at the onset of exercise
Movement of limbs has strong influence
3. Learned componentVentilation increases gradually
4. After immediate increase, gradual increase occurs (4-6 minutes)
Anaerobic threshold: highest level of exercise without causing significant change in blood pH. If exceeded, lactic acid produced by skeletal muscles
There are many possible complications in respiration.
Respiratory Complications
- Sudden Infant Death Syndrome (SIDS)
- Emphysema
- Pulmonary embolism
- Pneumonia
- Tuberculosis
- Cystic Fibrosis
Respiratory Help Mechanisms
- Heimlich maneuver
- Tracheotomy